This Client went Phasic in their Gait. Do you know what that means ? We do, and so does McGill, Liebenson, Cook and many others.
Long ago on this blog we showed and discussed a video (link) that discussed Stu McGill's research of the human movements of Georges St-Pierre and David Loiseau. The basic tenets of that video were that the hips and shoulders are used for power production and that the spine-core are used for creating stiffness and stability for the ultimate power transmission through the limb. He made it clear that if power is generated from the spine, it will suffer.
Here on TGG we have long talked about phasic and antiphasic motions of the arms and shoulder-pelvic blocks during gait and locomotion/sport activity. Many of our 1000+ blog writings and 80 podcasts have talked about spine pain and how spine pain clients reduce the antiphasic rotational (axial) nature of the shoulder girdle and pelvic girdle. In the video above, we see anything but antiphasic gait, to be clear, this is a classic representation of a phasic gait. This is pathologic gait, the frontal plane sway is exaggerated and necessary because there is no axial antiphasic motion. There is essentially frozen arm and torso movements. This client has a long standing history of severe spine trauma and pain, their central pattern generators (CPG) had to make this motor pattern choice in an attempt to avoid pain and negotiate force streams across trauma zones. If you are curious and wish to go deeper down this rabbit hole, read the 30+ articles we have produced more specifically on arm swing and locomotor phasics, just click here.
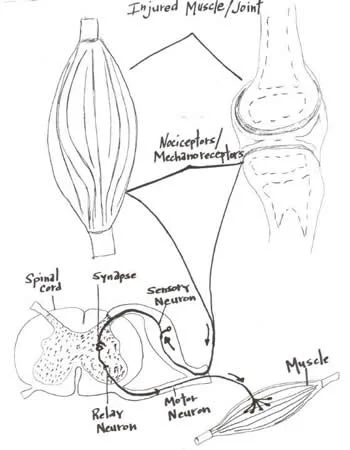
In these types of cases, the client subconsciously makes the subcortial pattern choice (overrides the normal CPG) to rotate them as a solid unit to reduce spine rotation, axial loading and compression. We could say that quite often spine pain disables the normal arm-leg pendulums via altering the shoulder-torso and hip-pelvis phasics and the CPG that dictates them. Normally, the spine and core must present sufficient amounts of recruited stiffness, yet mobility where necessary, to enable the locomotive power and velocity generated by movements of the shoulders and hips. These are the two main portals of limb movement off of the spine/core. These principles holds true in gait and sport. For and interesting example, in human gait the psoas is not entirely a hip flexor initiator when it comes to leg swing, it is a huge hip flexion perpetuator. The initial hip flexion in human gait comes from derotating the obliqued pelvis, via abdominal contraction, on a stiff and stable spine. Once the pelvis rotation is initiated, the femur can further pendulum forward (via contraction of the psoas and other muscles) on the forward accelerated pelvis in the hip joint proper creating an energy efficient movement (the towel flick/whip effect). This premise holds true in gait, running, kicking etc. This is a solid principle of effective and efficient human locomotion. This principle also holds true for a punch or throwing an object, the stable torso/spine provides a stable anchor upon which to accelerate the arm in order to create a high velocity limb movement with power. But here is where we get annoyed much of the time. (Soap box Tangent coming up) How often do you read articles about tight ITBand, tight psoas, tight piriformis and the like ? As a “diagnosis” these are weak and they are the “go to diagnosis or cause” of the unseasoned clinician, trainer, coach, therapist. If we all are to be really good at our job, we must go beyond what we see in someone’s gait (since it is the compensation) and go beyond the CNS neuroprotective strategy of tightness/shortness when there is weakness or motor pattern failure. This does not mean that you cannot, or should not, incorporate restoration methods and principles to restore length-tension relationships in your client, it means you have to resolve ALL of the problems, including the aberrant CPG they have set up as a protective default to avoid injury or further injury.
In the case above, returning the discussion to arm and leg swing, one must understand clearly that faulty arm swing patterns and lack of antiphasic torso and pelvis oscillation is a product of surgery, trauma and more so, pain. The client is avoiding the antiphasic presentation (hence, he is phasic) for a reason and coaching more arm swing would be just about the dumbest intervention, so don’t be “that guy”. We know this is an altered motor pattern choice, not a new fixed set point. We know this because on clinical examination the range is available, we know because we examined for it, it is just not being used. In an example of this same principle, in this case talking hip ranges of motion, McGill discusses the same in his paper*:
“Despite the large increases in passive hip ROM, there was no evidence of increased hip ROM used during functional movement testing. Similarly, the only significant change in lumbar motion was a reduction in lumbar rotation during the active hip extension maneuver (p < 0.05). These results indicate that changes in passive ROM or core endurance do not automatically transfer to changes in functional movement patterns. This implies that training and rehabilitation programs may benefit from an additional focus on grooving new motor patterns if newfound movement range is to be used.”
Think about that next time you stretch, or are stretched by someone. As we have said before, just because you increase someone’s range of motion, does not mean they will be able to incorporate that range of motion into a movement pattern, or compensation pattern for that matter. It is only ¼ of the equation: Range of Motion, Skill (or proprioception), Endurance (or the proportion of slow twitch muscle) and Strength (the proportion of fast twitch muscle). There is our S.E.S. mnemonic again.
In this video case, lack of NORMAL antiphasic spinal motion (torso and pelvis moving opposite one another) is noted. Without the obliqued pelvis the swing and stance phases will be impaired. The psoas may have to become more of a hip flexor initiator, AS WELL AS the perpetuator of limb swing, because there is no pelvic obliquity from the antiphasic principles to drive it from. And so, when you see this fella in your office with bilateral tight psoas/hip flexor complex and tight quadriceps mechanisms with resultant impaired glutes and hip extension, please do not begin lengthening them as your point of initiation. They are that way because he has gone phasic in his gait. Change the motor patterns that drive this as best as possible, restore any weaknesses that are contributory to, or initiate, these motor patterns and then, if needed, encourage some progressive new length-tension in these muscle groups as improved motor patterning evolve to allow for it. You are likely going to have to go back and reteach and restore primitive and postural sensory motor windows in these cases, so be patient, be kind, be wise. Oh, and do not forget that with impaired hip function, there will most likely be impaired ankle rocker, you are going to need a wide angled lens to see, capture and remedy this lads problems.
On another note, can you imagine what this client’s video gait analysis would show and interpret ? Let alone the diagnostics and recommendations that could come from it? What about the appearance of their foot pressures across a dynamic foot pressure plate (or God forbid a static one !), surely what is seen at the foot is this client’s problem (not !) And forgive those poor fools who recommend a shoe for this client based off of just those mediums alone. Without a complete hands-on clinical examination to correlate gait cycle observances, any recommendations for this case will be traumatic on many levels.
Today’s bottom line……. read, learn, think, stay hungry, be wise.
Shawn and Ivo, The Gait Guys
* Improvements in hip flexibility do not transfer to mobility in functional movement patterns. Moreside, Janice: McGill, Stuart