“Hey guys, I absolutely love the show, especially as it becomes less and less over my head.
Due to your love of gait-altering absurdly thick EVA midsoles, I thought you might like to check out this Hoka incident that occurred at the Marathon des Sable across the Sahara in Morocco, a 6 day 251km event. It was posted by Ian Corless at Talk Ultra Podcast. Apparently the medial side of the midsole collapsed–on DAY 2! This guy finished the race, and as you have to carry 100% of your gear and nutrition, I guess he only had the one pair. It looks like this runner should fly out to CO or IL asap, because if he didn’t have gait issues before, he is sure to have them now.”
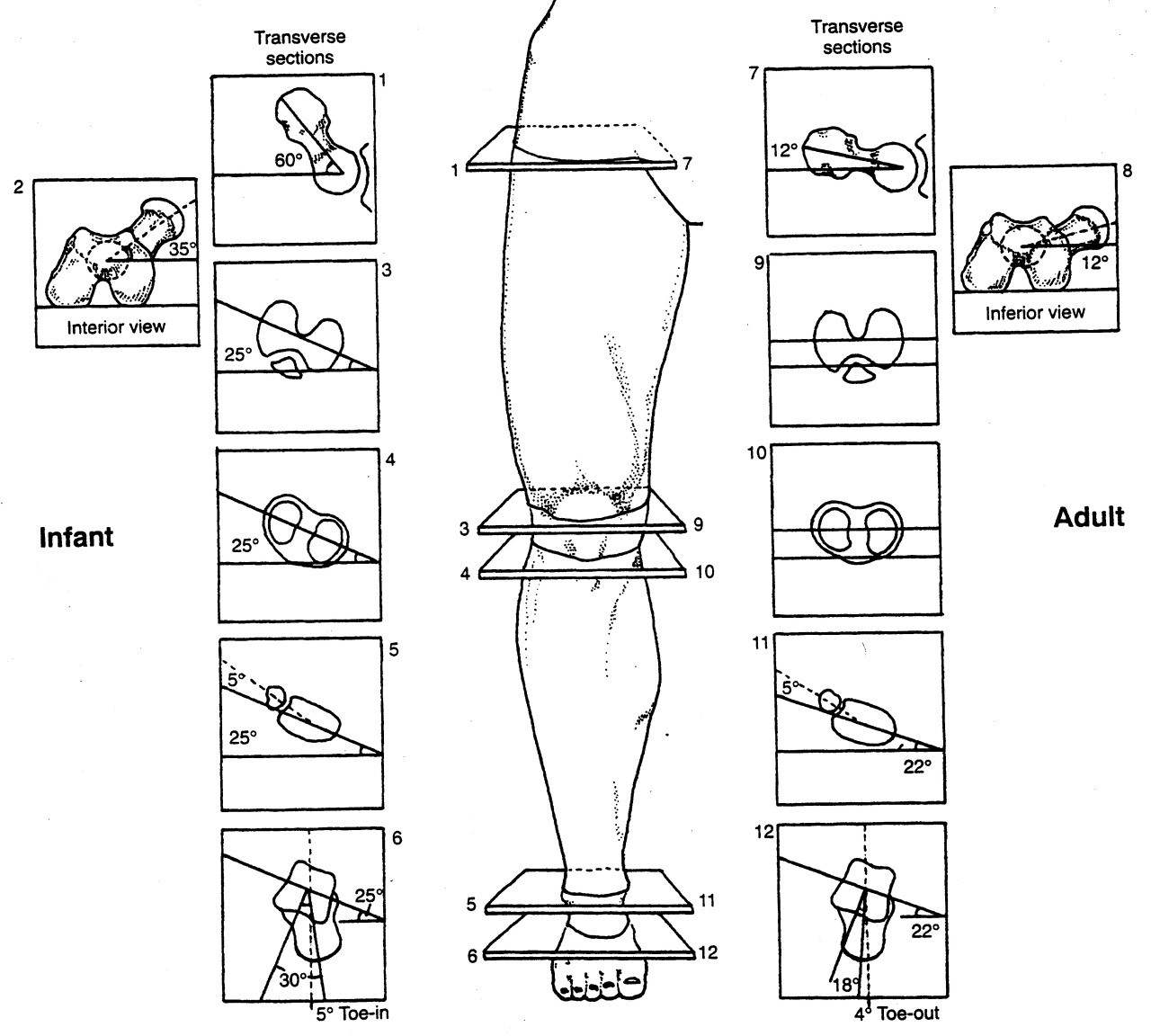
This brings up some scary thoughts when it comes to the amount of EVA foam and quality of foam (EVA or otherwise) being used in some shoes. "The more foam there exists, the greater one can break down into their compensation or deforming strategy.“ What do we mean by this ? Well, two things should be on one’s mind: 1. all foam breaks down into the vector of the deforming forces and 2. most of us do not have perfectly clean biomechanics, thus an abnormal loading vector is most likely present. These aberrant biomechanics are eventually reflected into our shoes as a "wear pattern”. In this case, the EVA foam had progressively broken down into their rearfoot pronation (and likely mid and forefoot pronation). In this case, even if the person had enough tibialis posterior and other medial pronation-decelerating structure strength at the start, the acceleration of their foot into this issue is now even more abrupt, brisk, excessive etc. A new pair of shoes would not be broken down into this deformity and so a newer pair of shoes is preventive. This is why we recommend new shoes often, and the cycling in of another pair (or several pair) into the mix so that one is never driving the same shoes into the potentially destructive compensation patterns that most of us have. At least with a fresh pair of shoes brought into the mix at the 200 mile wear point, you would only be in the more destructive shoes every other run, giving the body time to recuperate more.
As for this pair of shoes, this runner either has a terrible right foot problem or this was a brutally flawed right shoe from the get go, or both. We can only imaging how painful the medial knee might be at this point. Furthermore, imagine the abrupt nature of the hip internal rotation mechanics ! IF they do not have hip labrum impingement yet, they will soon ! And with that amount of internal limb spin, can you imagine how inhibited the glutes would be from constantly having to eccentrically control that excessive rotation?
As a whole, are not huge fans of the HOKA shoe family, we just cannot fathom the need for this much foam under the feet. If you have been with us long enough you will have heard on our podcast and blog talk about increased impact forces with increasing EVA foam thickness (want that info, here is the link and references). Just because some EVA foam is good, doesn’t mean more is better. Remember, to propulse off of a foam infrastructure you must bottom out/compress the foam sufficiently to find a firmness to propulse from. The Hoka’s have plenty of foam making this our concern, and we are not picking on just them. There are other companies doing this “super sizing/super stacking” such as Brooks, Altra, and New Balance to name just a few. Sure they have added a greater forefoot rocker/toe spring on the front of the shoe to help (they have to because the foam thickness is so great that there is no flexing of the forefoot of the shoes), but is it enough for you? Remember, every biomechanical phase of the gait cycle is necessary and timely to engage the natural joint, ligament, muscle components of joint loading, mobility, stability and movement. If you spend too much time in one phase (perhaps because you are waiting for foam to decompress) you may wait a moment too long and miss the opportunity for another critical phase to begin in the sequence. This is the root cause of many injuries, aberrant biomechanics leading to aberrant mobility or stability.
So remember these few things:
1. more is not always better for you, it may be for some, but maybe not you.
2. there is a price to pay somewhere in the mechanical system, after all the body is a contained system. What doesn’t happen at one joint often has to be made up at the next proximal or distal joint.
3. Everyone has some aberrant mechanics. No one is perfect. These imperfections will reflect in your shoes, and the longer you are in a pair of shoes the deeper the aberrant mechanics will be reflected in your shoe, thus acting as a steering wheel for the aberrant pattern (the steering is more direct/ more aggressive than in a new pair of shoes). So keep at least 2 pair of shoes rotating in your run cycle, one newer and one half done. We even recommend 3 pairs often. Trust us, the sudden biomechanical shift from a dead shoe into a new one (even though it is a clean new shoe without bad patterns in it) is still a biomechanical shift and could cause adaptive phase problems, pain or injury.
Lots to consider in this game. It is not just about dropping into barefoot and taking off down your street. Not if you want to be doing this for a long time and stay healthy.
Shawn and Ivo, the gait guys
* next day follow up from our social media pages:
Along the lines of EVA and yesterdays post:
“Wear of the EVA consistently increased heel pad stresses, and reduced EVA thickness was the most influential factor, e.g., for a 50% reduction in thickness, peak heel pad stress increased by 19%. ”
This study looks at a model; it would be interesting to see this study with a large cohort.
Role of EVA viscoelastic properties in the protective performance of a sport shoe: computational studies.
Even-Tzur N1, Weisz E, Hirsch-Falk Y, Gefen A.
http://www.ncbi.nlm.nih.gov/pubmed/17075164